In the United States, total health expenditure is around 16 percent of GDP, which is approximately 30 percent higher than at the beginning of the century, after adjusting for inflation. Despite the US having a strong and growing economy, the quality of health outcomes is uneven in areas such as primary care and avoidable hospital admissions, relative to other similar OECD countries.
In this context, the Affordable Care Act has introduced several policies aimed at achieving the best patient outcomes possible at the lowest cost. For example, healthcare providers receive bonuses for cutting costs and incur penalties for undesirable outcomes, such as patient readmission to hospitals after discharge. The Centers for Medicare and Medicaid Services (CMS) have implemented the Value Modifier, which adjusts physicians’ payments based on the quality and cost of the care provided. Moreover, in January 2015, the US Department of Health and Human Services (HHS) announced the goal of using alternative payment models to tie 90 percent of traditional fee-for-service payments to treatment quality by 2018.
In a recent study, researchers from Wisconsin-Madison, Yale, and NYU investigate how insights from education research can inform value-added models of physician care. In the education space, value-added measures help quantify the quality of teachers. These measures calculate teachers’ precise impact on student test scores, controlling for previous achievement and other contextual characteristics, such as students’ socioeconomic status.
To calculate the “physician effect,” or the value-added measure for each doctor, the researchers relate patients’ health at the time of discharge to their interaction with the physicians, controlling for patient characteristics, such as age and gender, and baseline health upon initial admission to the hospital. The study uses the Rothman Index to measure the health status of patients, with values ranging from -91 to 100, where higher values indicate better health. This index is calculated from vital signs, results of physical examinations, laboratory results, and nursing assessments of health status, among other indicators. Controlling for baseline health status prevents very sick patients from dragging down the value-added measures of their physicians, and allows the researchers to observe patients’ health trends relative to their initial health status.
Their data come from the billing and medical records of 16,187 medical and surgical inpatients admitted to Yale New Haven Hospital between July 1, 2011 and June 30, 2012. These patients were treated by 163 different attending physicians.
Physicians were ranked according to value-added scores, from low to high quality, which turned out to be highly stable over the course of the study. These metrics identified the most and least effective physicians but did not give information regarding the reasons behind these differing impact levels. On average, patients of physicians in the highest quartile of value-added measures experienced a shorter average stay in the hospital (4.76 days) relative to patients of physicians in the lowest quartile (5.08 days). Patients of top-quartile physicians also ended up paying lower average costs ($17,811) relative to patients of bottom-quartile physicians ($19,822). Patients of top-quartile physicians were in better health at the time of discharge from the hospital. These differences between patients of top- and bottom-quartile physicians are summarized in the chart below.
These value-based measures can improve efforts to maximize value for patients, as they can lead to a more efficient allocation of resources towards high-quality physicians. However, these measures also have some shortcomings. This methodology does not capture the effect of care provided by other medical professionals, such as nurses. Rather, all improvement in a patient’s status is attributed to the main physician. In the future, the model and methodology could be extended to include nurses and other staff members, to measure and control for their effects. Larger databases, with information on more hospitals across the country, could also extend the power of this analysis and generate value-added measures at the hospital level.
Composite measures of effectiveness, which include value-added measures in addition to other variables, can often be more informative than value-added measures alone. For example, a composite measure of physician effectiveness could include reported patient satisfaction levels in addition to the value-added measures outlined here. Developing robust measurements of physician performance can help improve efficiency in the health sector and inform important decisions about compensation and retention in our nation’s hospitals.
Article Source: Fletcher, Jason M., Leora I. Horwitz, and Elizabeth Bradley, “Estimating the Value Added of Attending Physicians on Patient Outcomes,” National Bureau of Economic Research. October 2014.
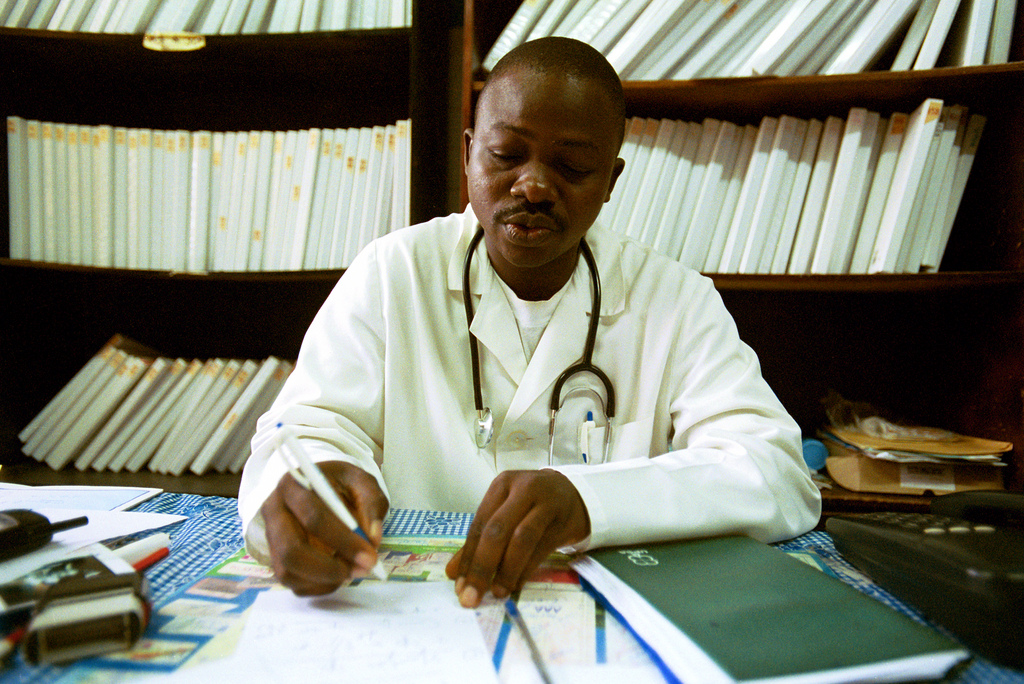
Featured Photo: cc/(World Bank Photo Collection)